Welcome ! Bienvenue! Bienvenido! Bun Venit! ようこそ (Yōkoso)
Wound Infections After Surgery
How to Prevent Wound Infections After Surgery. Surgical wounds are a critical part of the recovery process and must be handled with meticulous care to avoid complications. A surgical wound infection, or surgical site infection (SSI), can occur when harmful bacteria invade the incision site.
NURSING BLOG
Mihaela Schmitz, LVN
12/10/20243 min read
Surgical wounds are a critical part of the recovery process and must be handled with meticulous care to avoid complications. A surgical wound infection, or surgical site infection (SSI), can occur when harmful bacteria invade the incision site. These infections can lead to delayed healing, systemic complications, and even hospital readmission. As a highly experienced wound care nurse, I’ve seen how the right post-operative care can significantly reduce these risks. Below, I’ll provide an in-depth guide to preventing wound infections, blending medical terminology with clear explanations to empower patients and caregivers alike.
1. Understand the Risk Factors for Surgical Site Infections (SSIs)
Certain factors increase the likelihood of developing an SSI. These include comorbidities like diabetes or obesity, poor nutritional status, smoking, and inadequate wound care. Patients undergoing procedures with large or deep incisions, such as an abdominal laparotomy or hip replacement, are particularly vulnerable. Knowing these risks allows patients and caregivers to be more vigilant during recovery.
2. Adhere to Post-Operative Instructions Precisely
Surgeons and nurses provide tailored post-operative instructions for a reason: they are designed to minimize complications. These guidelines might include how to clean the wound, when to change dressings, and what activities to avoid. For example, patients recovering from abdominal surgery are often advised to limit heavy lifting to prevent dehiscence (wound reopening), which could introduce bacteria.
3. Practice Strict Hand Hygiene Before Wound Care
Proper hand hygiene is essential to prevent bacterial transfer to the surgical site. Use antibacterial soap and warm water to wash your hands thoroughly for at least 20 seconds. In medical settings, we often use an alcohol-based hand rub (ABHR) as an additional layer of disinfection. For caregivers, wearing sterile gloves during dressing changes adds another level of protection.
4. Maintain a Clean and Dry Wound Environment
Bacteria thrive in moist, warm environments. Surgical wounds should remain clean and dry unless advised otherwise by your healthcare provider. During cleaning, use a normal saline solution or an antimicrobial cleanser, as these are gentle on tissues while reducing bacterial load. Avoid submerging the wound in water, such as baths or pools, until it’s fully healed, as stagnant water can harbor pathogens.
5. Change Dressings According to Medical Guidelines
Dressings act as a physical barrier to bacteria. Occlusive dressings, which create a sealed environment, are often used for surgical wounds to promote healing and protect against infection. However, if the dressing becomes soaked or soiled, it should be replaced immediately to prevent microbial colonization (the buildup of bacteria on the wound surface). Follow your nurse or doctor’s recommendations for frequency and technique.
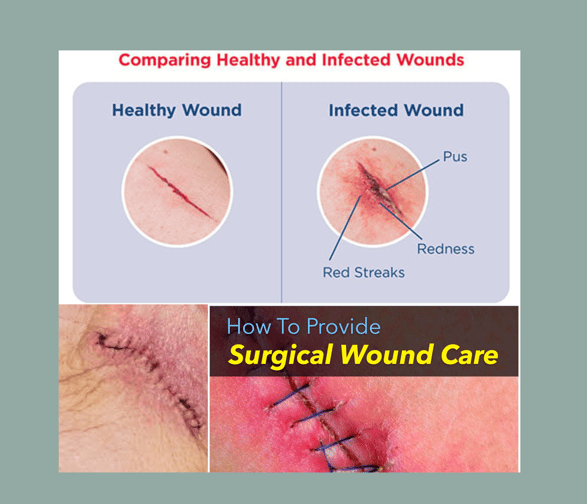
6. Recognize the Signs and Symptoms of Infection Early
Early detection of infection is crucial for effective treatment. Look for:
Erythema (redness) spreads around the wound.
Excessive swelling or warmth at the incision site.
Purulent drainage (pus) with a yellow, green, or foul-smelling discharge.
Fever or chills, which may indicate a systemic infection.
If any of these signs occur, contact your healthcare provider immediately to prevent escalation to sepsis, a life-threatening condition.
7. Optimize Nutrition for Wound Healing
A balanced diet rich in protein, vitamins A and C, and zinc supports tissue repair. Protein, found in lean meats, fish, and legumes, is essential for collagen synthesis, a key process in wound healing. Vitamin C strengthens the immune system and promotes new blood vessel formation, or angiogenesis, ensuring oxygen and nutrients reach the healing tissues.
8. Eliminate Habits That Impair Healing
Smoking significantly reduces oxygen flow to the wound by constricting blood vessels, a process known as vasoconstriction. This slows healing and increases infection risk. Similarly, alcohol weakens the immune system, leaving the wound susceptible to bacterial invasion. Eliminating these habits, even temporarily, can make a measurable difference in recovery.
9. Attend All Follow-Up Appointments
Post-operative follow-ups allow your healthcare provider to assess wound healing and intervene early if issues arise. During these visits, your doctor or nurse may evaluate for granulation tissue—a sign of healthy healing—or check for signs of delayed healing or infection. Skipping these appointments increases the risk of undetected complications.
10. Choose Skilled Wound Care Professionals
Wound care is a specialized field that requires both technical expertise and a compassionate touch. Skilled nurses, like myself, bring years of training to ensure wounds are cleaned, dressed, and monitored for complications. I dedicate the time needed to deliver exceptional care. My services are tailored to your unique needs and provided in the comfort of your home, ensuring privacy and convenience.
Conclusion
Preventing wound infections after surgery is a collaborative effort that involves patients, caregivers, and skilled healthcare providers. By adhering to these evidence-based practices, you can minimize your risk and ensure optimal healing. If you need personalized wound care, reach out to Mihaela Nursing Services. With expert care and unwavering commitment, I’ll guide you through a safe and successful recovery.
Contact Mihaela Nursing Services today to schedule a consultation.
Coming Soon Subscribe to our Gazette:
Copyright © Mihaela's Nursing Services. All Rights Reserved.
Service Area: Goleta, Santa Barbara, Montecito
Nurse Mia is doing home visits
Hours
Monday - Friday
8:30 - 17:00
Weekends by appointment
* leave a voicemail or text - I can't answer while I am with a patient, but usually, ETA is 1.5 hours -during working hours


